West Texas #1 Dry Eye Treatment Center
dry eye testing
Meibography
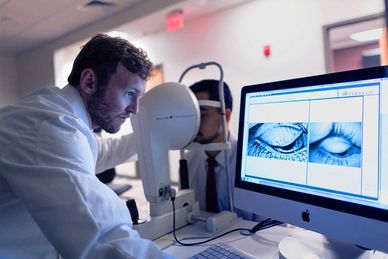
A meibography visualizes the morphology of the meibomian glands through a series of high-definition digital images. The images allow the eye doctor to observe the architecture of the glands by revealing the gland size, structure, and any structural abnormalities.
Inflammatory MMP-9 Markers
MMP-9 is an inflammatory biomarker that has been shown to be elevated in the tears of patients with dry eyes. The authors administered an immunoassay test called InFlammaDry on 143 patients with clinical signs and symptoms of dry eye confirmed by clinical examination and 63 healthy individuals serving as controls. The test is designed to detect abnormally elevated MMP-9 present in the late phase of the inflammation cycle and therefore may be more clinically relevant than causal mechanisms or acute symptoms. The results are available in 10 minutes. InflammaDry showed a sensitivity of 85 percent, specificity of 94 percent, negative-predictive value of 73 percent, and positive predictive value of 97 percent. False-negatives occurred uniformly across all levels of dry-eye severity, which suggests they may have been the result of inadequate collection and transfer of tear samples. Although MMP-9 activity is elevated in symptomatic dry eyes, as well as in other clinically easily identifiable ocular surface conditions, InflammaDry also reveals asymptomatic ocular surface disease and the hidden inflammation of dry eyes. The authors say that patients with positive test results with InflammaDry may benefit from treatment with anti-inflammatory therapy, while those with negative results and a positive clinical examination may have dry eye without significant accompanying inflammation and may benefit from artificial tear replacement or punctal occlusion. If artificial tears are ineffective at relieving symptoms, a therapeutic trial of anti-inflammatory therapy to target subclinical inflammation may be necessary. They conclude that the ability to accurately detect elevated MMP-9 levels may lead to earlier diagnosis, more appropriate treatment and better management of ocular surface disease.
Corneal Topography

Missing or patchy information on topography is often an indicator of early tear break-up time (TBUT). Inferior steepening is also a common result of dry eye, which can become so severe as to mimic keratoconus. The inferior cornea will often steepen in dry eye because of epithelial dehydration.
TEARLAB™ OSMOLARITY

The TearLab Osmolarity Test Card, in conjunction with the TearLab Osmolarity System, provides a quick and simple method for determining tear osmolarity using nanoliter (nL) volumes of tear fluid collected directly from the eyelid margin. The Test Card is held by the Osmolarity Test Pen, for safe collection.
Tear osmolarity as a diagnostic tool. Evaluating the diagnostic ability of tear osmolarity requires specifying a value that discriminates a healthy eye from an eye with DED; this value is known as the threshold value. In the literature, tear osmolarity threshold values have varied from 305 mOsm/L8 to 316 mOsm/L
What is Tear Osmolarity? Put simply, tear osmolarity is a measurement used to determine how much salt is in your tears. Normal osmolarity is essential for proper tear production, retention, distribution, and elimination. When your tears have too much salt in them, it's called hyperosmolarity.
Normal tear film is in homeostasis with blood osmolarity at a reference value of 290 mOsm/L, with a normal "homeostatic range" for tear osmolarity defined as 275-307 mOsm/L.
The normal pH range was 6.5 to 7.6; the mean value was 7.0.
Tear Break Up Time

TBUT (Tear Break Up Time)
Tear film continuity is maintained by blinking. If a person keeps their eyes open long enough, without blinking, their tear film will start breaking up.
This makes the eye feel uncomfortable and forces you to blink to maintain comfort. In patients with dry eyes, the tear film is unstable and tends to break up faster. Therefore the tear break up time in patients who have dry eyes is shorter.
Generally, >10 seconds is thought to be normal,(10, 11, 12) 5 to 10 seconds, marginal, and < 5 seconds is considered low. A short tear break-up time is a sign of a poor tear film and the longer it takes the more stable the tear film.
These stains are the most diagnostic for early to moderate dry eye. When evaluating the interpalpebral conjunctiva, positive staining with lissamine green helps to detect the earliest signs of the disease prior to corneal staining. Lissamine green is the vital dye of choice used in symptomatic patients who have not yet started to show corneal fluorescein staining.
SCHIRMER TESTING

The Schirmer’s test is used determine if your tear glands produce enough tears to keep your eyes adequately moist. Calibrated strips of a non-toxic filter paper are used. One free end is placed within your lower eyelid. Both eyes are tested at the same time. Before the test, you may be given numbing eye drops to prevent your eyes from tearing due to irritation from the paper. You will be asked to keep your eyes gently closed for 5 minutes. At the conclusion of the test, the paper strips are removed from each lower eyelid and the amount of wetting of the paper strips is measured. Wetting of less than 5 mm is indicative of deficient tear production, but is not necessarily diagnostic of Sjögren’s syndrome. The results need to be correlated with other findings on the eye exam in order to determine if you have a dry eye syndrome.
A normal level of production is considered to be over 10 millimeters (mm) of tears on the paper. Anything under 10 mm is considered to be an abnormally low level of tear production. A measurement of less than 5 mm is considered severe dry eye.
ROSE BENGAL STAINING
ROSE BENGAL STAINING
ROSE BENGAL STAINING
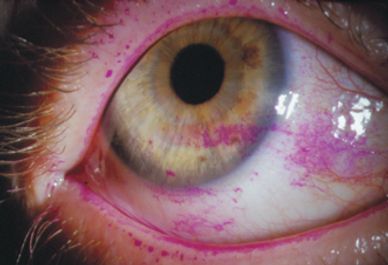
Rose bengal staining is analogous to lissamine green, but because it can burn upon instillation, it is used less than its green-colored counterpart. Unlike fluorescein and lissamine green, rose bengal staining is not a “vital” dye, as it stains normal, healthy, living cells in addition to dead or dying ones.
Stains dead and devitalised cells including mucous strands on ocular surface.
The stain is taken up wherever there is deficiency of preocular tear film protection, thereby helping in the diagnosis of ocular surface disorders.
Uses
Conjunctival staining:
Diagnosis of dry eye disease
Dysplastic or squamous metaplastic cells of conjunctival squamous neoplasms
Corneal staining for herpetic corneal epithelial dendrites, superficial punctate keratitis.
Diagnosis of Meibomian gland dysfunction.
Superior to other stains for early detection of ocular surface disorders.
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.